Our Vision
"To empower individuals worldwide with accurate, accessible, and compassionate medical knowledge, fostering informed decisions and healthier lives. We strive to be a trusted source of evidence-based health information, bridging the gap between medical expertise and everyday wellness, while inspiring a global community to prioritize prevention, education, and holistic well-being."
Our Mission
Through evidence-based content, expert insights, and practical advice, we aim to educate, inspire, and support our readers in making informed health decisions. We are committed to promoting wellness, preventing disease, and fostering a culture of health literacy, ensuring that everyone has access to the knowledge they need to live healthier, more fulfilling lives.".
Dandruff


Scalp dandruff is a common condition characterized by flaking of the skin on the scalp. It is often accompanied by itching and can be embarrassing or uncomfortable.
1. Symptoms of Scalp Dandruff
- White flakes: Visible flakes of dead skin on the scalp and hair.
- Dryness: The scalp may feel dry and tight.
- Redness or irritation*: In some cases, the scalp may become inflamed, with persistent itching of the scalp.
2. Causes of Scalp Dandruff*
- Seborrheic dermatitis: A common cause, linked to an overgrowth of a yeast-like fungus called Malassezia fur fur, which is the common culprit.
- Dry skin: Flakes from dry skin are typically smaller and less oily.
- Oily skin (seborrhea): Overactive oil glands can lead to dandruff.
- Poor hygiene: Infrequent shampooing can lead to buildup of oil and skin cells.
- Sensitivity to hair products: Certain shampoos, conditioners, or styling products can irritate the scalp.
- Skin conditions: Psoriasis, eczema, or fungal infections can cause flaking.
- Diet and stress: Poor nutrition or high stress levels may worsen dandruff.
- Climate: Cold, dry weather can exacerbate dandruff.
3. Types of Dandruff
- Dry skin-related dandruff: Small, white flakes caused by dry scalp.
- Oily skin-related dandruff: Larger, yellowish flakes caused by excess oil and Malassezia overgrowth.
- Fungal dandruff: Caused by fungal infections like *Malassezia.
- Psoriasis or eczema-related dandruff: Flakes caused by underlying skin conditions.
4. Diagnosis
- Visual examination: A doctor or dermatologist can usually diagnose dandruff by examining the scalp.
- Skin scraping with KOH: In rare cases, a sample may be taken to rule out fungal infections or other conditions.
5. Treatment and Management
Over-the-Counter Treatments*
- Anti-dandruff shampoos: Look for active ingredients like:
- Zinc pyrithione: Reduces fungus and bacteria.
- Ketoconazole: Antifungal agent.
- Selenium sulfide: Slows skin cell turnover and reduces fungus.
- Salicylic acid: Exfoliates and removes flakes.
- Coal tar: Slows skin cell growth and reduces flaking particularly useful in psoriasis of scalp.
- Moisturizing shampoos: For dry skin-related dandruff.
Prescription Treatments
- Stronger antifungal shampoos or creams: For severe cases.
- Topical steroids: To reduce inflammation and itching.
Home Remedies
- Tea tree oil: Has antifungal and antibacterial properties.
- Apple cider vinegar: Helps balance scalp pH and reduce fungus.
- Coconut oil: Moisturizes the scalp and reduces dryness.
- Aloe vera: Soothes irritation and reduces flaking.
Lifestyle Changes
- Regular shampooing: Keeps the scalp clean and reduces oil buildup.
- Avoid harsh hair products: Use gentle, fragrance-free products.
- Balanced diet: Include foods rich in zinc, B vitamins, and omega-3 fatty acids.
- Stress management: Practice relaxation techniques to reduce stress.
6. Prevention
- Maintain scalp hygiene: Wash your hair regularly with a mild shampoo.
- Avoid excessive heat styling: Heat can dry out the scalp.
- Stay hydrated: Drink plenty of water to keep your skin hydrated.
- Limit hair products: Avoid heavy gels, sprays, or waxes that can build up on the scalp.
- Protect your scalp: Wear a hat in extreme weather conditions.
7. When to See a doctor
- If dandruff persists despite using over-the-counter treatments.
- If the scalp becomes red, swollen, or painful.
- If there are signs of infection (e.g., pus, bleeding, or severe itching).
8. Complications
- Hair loss: Scratching or inflammation can damage hair follicles.
- Social embarrassment: Visible flakes can affect self-confidence.
- Secondary infections: Scratching can lead to bacterial or fungal infections.
Scalp dandruff is a manageable condition, good sleep and healthy eating habits are key to success.
Eczema-


Eczema, also known as atopic dermatitis, is a common skin condition characterized by inflamed, itchy, and often red patches of skin.
It can vary in severity and often occurs in flare-ups. There are two types of eczema broadly speaking wet and dry, wet is characterize by oozing fluid.
1. Symptoms of Eczema
- *Itching: Intense itching is the most common symptom, often worsening at night.
- Dry skin: The affected skin may appear dry, scaly, or cracked.
- Redness and inflammation: Patches of skin may become red or swollen.
- Rashes: Common in areas like the face, hands, elbows, knees, and feet.
- Blisters or oozing: In severe cases, the skin may blister or leak fluid.
- Thickened skin: Chronic eczema can lead to thickened, leathery skin.
2. Types of Eczema
- Atopic dermatitis: The most common form, often linked to allergies and asthma.
- Contact dermatitis: Caused by exposure to irritants or allergens.
- Dyshidrotic eczema: Small blisters on hands and feet.
- Nummular eczema: Coin-shaped patches of irritated skin.
- Seborrheic dermatitis: Affects oily areas like the scalp and face.
- Stasis dermatitis: Linked to poor circulation, often in the lower legs.
3. Causes and Triggers
- Genetics: A family history of eczema, asthma, or allergies increases risk.
- Immune system overactivity: The immune system may overreact to irritants or allergens.
- Environmental factors: Dry weather, pollution, or exposure to harsh chemicals.
- Allergens: Pollen, pet dander, dust mites, or certain foods.
- Irritants: Soaps, detergents, synthetic fabrics, or perfumes.
- Stress: Emotional stress can worsen symptoms.
- Skin barrier dysfunction: A weakened skin barrier allows moisture to escape and irritants to enter.
4. Diagnosis
- Physical examination: A doctor examines the skin and reviews medical history.
- Patch testing: To identify potential allergens.
- Skin biopsy: Rarely, a small skin sample may be taken to rule out other conditions.
5. Treatment and Management
Major principle when dry make it wet, when wet make it dry.
- Moisturizers: Regular use of emollients to keep the skin hydrated.
- Topical corticosteroids: To reduce inflammation and itching.
- Antihistamines: To relieve itching, especially at night.
- Topical calcineurin inhibitors: Non-steroidal creams for sensitive areas.
- Phototherapy: Controlled exposure to UV light for severe cases.
- Systemic medications: Oral or injectable drugs for severe eczema (e.g., biologics like dupilumab).
- Lifestyle changes: Avoiding triggers, wearing soft fabrics, and managing stress.
6. Prevention
- Avoid triggers: Identify and avoid irritants or allergens.
- Maintain skin hydration: Use fragrance-free moisturizers daily.
- Gentle skincare: Use mild soaps and avoid hot showers.
- Humidify the air: Use a humidifier in dry climates.
- Dietary adjustments: Some people find relief by avoiding certain foods (e.g., dairy, nuts).
7. Complications
- Skin infections: Scratching can lead to bacterial or viral infections.
- Sleep disturbances: Itching can disrupt sleep.
- Mental health issues: Chronic eczema may lead to anxiety or depression.
8. When to See a doctor
- If symptoms are severe or not improving with over-the-counter treatments.
- If the skin becomes infected (e.g., pus, swelling, or fever).
- If eczema interferes with daily life or sleep.
The impact of shampoo on hair health.


The impact of shampoo on hair health.
The word shampoo entered the English language from the Indian subcontinent during the colonial era. It dated to 1762 and was derived from the Hindi word cā̃pō (चाँपो, itself derived from the Sanskrit root chapati (चपति), which means 'to press, knead, or soothe'.
Sake Dean Mahomed, an Indian traveller, surgeon, and entrepreneur, is credited with introducing the practice of shampoo or "shampooing" to Britain. In 1814, Mahomed, with his Irish wife Jane Daly, opened the first so called spa. In 1900, German perfumer and hair-stylist Josef Wilhelm Rausch developed the first liquid hair washing soap and named it "Champooing" in Emmishofen, Switzerland. Later, J.W. Rausch developed an antiseptic chamomile shampooing with a pH of 8.5.
In 1927, liquid shampoo was improved for mass production by German inventor Hans Schwarzkopf in Berlin; his name became a shampoo brand sold in Europe.
Originally, soap and shampoo were very similar products; both containing the same naturally derived surfactants, a type of detergent. Modern shampoo as it is known today was first introduced in the 1930s with Drene, the first shampoo using synthetic surfactants instead of soap.rcial "shampooing" vapour masseur bath in England, in Brighton.
Shampoo can have both positive and negative impacts on hair health, depending on its ingredients, frequency of use, and hair type. Here’s a breakdown of its effects:
Positive Impacts of Shampoo:
Cleanses the Scalp & Hair
Removes dirt, sweat, excess oil (sebum), and product buildup, preventing clogged hair follicles.
Reduces scalp irritation and dandruff caused by microbial growth (bacteria/fungi).
Improves Hair Appearance
Makes hair look fresh, shiny, and voluminous by removing greasiness.
Some shampoos contain conditioning agents that smooth the hair cuticle.
Treats Specific Scalp/Hair Issues
Medicated shampoos (e.g., ketoconazole, zinc pyrithione) help with dandruff, psoriasis, or seborrheic dermatitis.
Clarifying shampoos remove hard water minerals and heavy product residues.
Sulfate-free shampoos are gentler for color-treated or dry hair.
Negative Impacts of Shampoo:
Strips Natural Oils
Harsh surfactants (like sulfates: SLS, SLES) can over-cleanse, leading to dryness, frizz, and breakage, especially in curly or coarse hair.
Causes Scalp Irritation
Synthetic fragrances, parabens, and alcohol in some shampoos may cause allergic reactions, itching, or redness.
Damages Color-Treated Hair
Sulfates can fade hair dye faster, while certain shampoos may not protect color longevity.
Leads to Product Buildup
Silicones (e.g., dimethicone) in some shampoos can accumulate, making hair limp and dull over time.
Disrupts Scalp Microbiome
Over-washing can strip beneficial oils, disrupting the scalp’s natural pH balance and leading to oil overproduction (greasy roots) or dryness.
How to Choose the Right Shampoo for Hair Health:
For Dry/Damaged Hair: Use sulfate-free, moisturizing shampoos with oils (argan, coconut) or hyaluronic acid.
For Oily Hair: Look for clarifying shampoos (but don’t overuse) or gentle foaming cleansers.
For Color-Treated Hair: Opt for sulfate-free, color-safe formulas with UV protection.
For Curly/Coily Hair: Creamy, hydrating shampoos with shea butter or glycerine work best.
For Dandruff: Use anti-fungal shampoos (e.g., Nizoral, Head & Shoulders) 1–2 times weekly.
Best Practices to Minimize Damage:
Wash hair 2–3 times a week (adjust based on scalp oiliness).
Use lukewarm water (hot water strips moisture).
Follow with a conditioner to replenish moisture.
Occasionally use a deep-conditioning mask or pre-shampoo oil treatment.
Avoid shampoos with harsh sulfates, alcohol, or synthetic fragrances if sensitive.
Psychological aspects of psoriasis


The links between psoriasis and stress are complex. There are research articles proposing a review of the literature on the relationship between stress and psoriasis.
In 31-88% of cases, patients report stress as being a trigger for their psoriasis. There was also a reported higher incidence of psoriasis in subjects who had a stressful event the previous year, suggesting that stress may have a role in triggering the disease in predisposed individuals.
Stress is also a consequence of psoriasis outbreaks. Understanding the role of stress makes it appropriate to target stress when proposing treatment to patients with psoriasis.
Several controlled studies have demonstrated that relaxation, hypnosis, biofeedback, and behavioral and cognitive stress management therapies have been effective in people with psoriasis.
Psoriasis is a "mind-skin" condition—its psychological burden is as significant as its physical symptoms. Addressing mental health alongside medical treatment leads to better overall outcomes.
Emotional and Mental Health Impact
Depression & Anxiety:
Studies show that people with psoriasis are 1.5–2 times more likely to experience depression and anxiety than the general population.
The stress of flare-ups can trigger or worsen these conditions.
Low Self-Esteem & Body Image Issues:
Visible plaques (especially on the face, hands, or scalp) can lead to embarrassment, shame, and social withdrawal.
Some individuals avoid swimming, dating, or wearing certain clothes due to self-consciousness.
Anger & Frustration:
The chronic, incurable nature of psoriasis can lead to feelings of helplessness and anger.
Flare-ups may seem uncontrollable, causing distress.
Social & Behavioral Effects
Social Isolation & Stigma:
Fear of judgment or misunderstanding leads some to avoid social interactions.
Misconceptions (e.g., "it’s contagious") can result in discrimination or bullying.
Impact on Relationships & Intimacy:
Psoriasis in sensitive areas (scalp, genitals) may cause discomfort during physical intimacy.
Partners may lack understanding, leading to emotional distance.
Work-Related Stress:
Visible psoriasis can affect professional confidence and job performance.
Some report workplace discrimination or difficulty due to chronic symptoms (itching, pain).
Stress & the Psoriasis Cycle
Stress as a Trigger: Emotional stress is a well-known trigger for psoriasis flare-ups.
Vicious Cycle:
Psoriasis → Stress → Flare-up → More Stress → Worsening Psoriasis
Breaking this cycle is key to management.
Coping Mechanisms & Psychological Support
Therapy & Counselling:
Cognitive Behavioral Therapy (CBT) helps manage stress, negative thoughts, and coping strategies.
Support groups reduce feelings of isolation.
Mindfulness & Relaxation Techniques:
Meditation, yoga, and deep breathing can lower stress-induced flare-ups.
Open Communication:
Educating friends, family, and coworkers about psoriasis reduces stigma.
Medical & Holistic Approaches:
Treating psoriasis effectively (topicals, biologics, phototherapy) improves mental health.
Some benefit from antidepressants or anti-anxiety meds if mood disorders are severe.
Photo-aging


Photoaging or photoaging (also known as "dermatophilosis" is a term used for the characteristic changes to skin induced by chronic UVA and UVB exposure.
Effects of UV light
Molecular and genetic changes
UVB rays are a primary mutagen that can only penetrate through the epidermal (outermost) layer of the skin and can cause DNA mutations. These mutations arise due to chemical changes within skin cells. These mutations may be clinically related to specific signs of photoaging such as wrinkling.
DNA UV mutation
Melanocytes and basal cells are embedded in the epidermal layer. Upon exposure to UVB rays, melanocytes will produce more melanin, a pigment that gives skin its color. UVB can cause the formation of freckles and dark spots, both of which are symptoms of photoaging; these are most common in people with fair or light skin. With frequent long-term exposure to UVB rays, signs of photoaging might appear and precancerous lesions or skin cancer may develop.
UVA rays are able to penetrate deeper into the skin than UVB rays, damaging the dermal layer as well as the epidermal. The dermis is the second major layer of the skin and it comprises collagen, elastin, and extrafibrillar matrix which provides structural support to the skin.
However, with constant UVA exposure, the size of the dermis layer will be reduced, thereby causing the epidermis to start drooping off the body. Due to the presence of blood vessels in the dermis, UVA rays can lead to dilated or broken blood vessels which are most commonly visible on the nose and cheeks. UVA can also damage DNA indirectly through the generation of reactive oxygen species (ROS), which include superoxide anion, peroxide and singlet oxygen. These ROS damage cellular DNA as well as lipids and proteins.
Pigmentation
UV exposure can also lead to inflammation and vasodilation which is clinically manifested as sunburn. UV radiation activates the transcription factor, NF-κB, which is the first step in inflammation. NF-κB activation results in the increase of proinflammatory cytokines, for example: interleukin 1, IL-6 vascular endothelial growth factor, and tumour necrosis factor (TNF-α). This then attracts neutrophils which lead to an increase in oxidative damage through the generation of free radicals.
Additionally, UV radiation would cause the down-regulation of an angiogenesis inhibitor, thrombospondin-1, and the up-regulation of an angiogenesis activator which is platelet-derived endothelial cell growth factor, in keratinocytes. These enhance angiogenesis and aid in the growth of UV-induced neoplasms.
Immunosuppression
It has been reported that UV radiation leads to local and systemic immunosuppression, due to DNA damage and altered cytokine expression. This has implications in cutaneous tumour surveillance. The Langerhans cells may undergo changes in quantity, morphology, and function due to UV exposure and may eventually become depleted. One proposed explanation for this immunosuppression is that the body is attempting to suppress an autoimmune response to inflammatory products resulting from UV damage.
Degradation of collagen
UV exposure would also lead to the activation of receptors for epidermal growth factor, IL-1, and TNF-α in keratinocytes and fibroblasts, which then activates signalling kinases throughout the skin via an unknown mechanism. The nuclear transcription factor activator protein, AP-1, which controls the transcription of matrix metalloproteinases (MMP), is expressed and activated. MMP-1 is a major metalloproteinase for collagen degradation. This entire process is aided by the presence of reactive oxygen species that inhibits protein-tyrosine phosphatases via oxidation, thereby resulting in the up-regulation of the above-mentioned receptors. Another transcription factor NF-κB, which is also activated by UV light, also increases the expression of MMP-9.
In addition, the presence of damaged collagen would also down-regulate the synthesis of new collagen. The impaired spreading and attachment of fibroblasts onto degraded collagen could be one of the contributing factors to the inhibition of collagen synthesis.
Retinoic acids and photodamage
UV radiation decreases the expression of both retinoic acid receptors and retinoid X receptors in human skin, thereby resulting in a complete loss of the induction of RA-responsive genes. It also leads to an increase in activity of the AP-1 pathway, increasing MMP activity and thus resulting in a functional deficiency of vitamin A in the skin.
Signs, symptoms and histopathology
Early symptoms of photoaging:
Dyspigmentation, the formation of wrinkles and other symptoms appear around regions of skin commonly exposed to sun, mostly the eyes, mouth and forehead. The lips may be affected. In Canadian women, the upper chest is commonly affected.
Spider veins on face and neck
Loss of colour and fullness in lips
Symptoms of photoaging attributed to prolonged exposure to UV:
Wrinkles deepen and forehead frown lines can be seen even when not frowning.
Telangiectasias (spider veins) most commonly seen around the nose, cheeks and chin.
Skin becomes leathery and laxity occurs.
Solar lentigines (age spots) appear on the face and hands.
Possibly pre-cancerous red and scaly spots (actinic keratoses) appear.
Cutaneous malignancies
In addition to the above symptoms, photoaging can also result in an orderly maturation of keratinocytes and an increase in the cell population of the dermis where abundant; hyperplastic, elongated and collapsed fibroblasts and inflammatory infiltrates are found.
Photodamage can also be characterized as a disorganization of the collagen fibrils that constitute most of the connective tissue, and the accumulation of abnormal, amorphous, elastin-containing material, a condition known as actinic elastosis.
Epidermal thickness
UV exposure which would lead to an increase in epidermal thickness could help protect from further UV damage.
Pigment
It has been reported in many cases that fairer individuals who have lesser melanin pigment show more dermal DNA photodamage, infiltrating neutrophils, keratinocyte activation, IL-10 expression and increased MMPs after UV exposure.
Challenges in using Sun protection products.


Since time immemorial, people protected themselves from solar radiation.
Limiting time in the sun by seeking shade or wearing clothing was a matter of course. In the early 20th century, tanned skin – a result of exposure to sunlight – was associated with good health.
At the same time, however, one also had to protect oneself against the potential of excessive exposure to avoid sunburns.
Around 1945, the first sunscreen products for protection against solar radiation became available. In the years to follow and up to the recent past, a vast number of different sunscreen filters were developed and incorporated into a wide variety of product formats.
It was initially promoted as a lifestyle product and had the task of preventing sun-related erythema (tan without burn). Later, the prevention of skin cancer was added. Only in recent times, sunscreen products have been increasingly advertised and perceived as beauty and lifestyle products again.
Also, the use of sunscreen products for antiaging purposes is now commonplace. The different intended purposes (averting harm and prevention) and the widespread use of topical sunscreen products have promoted many investigations and generated a vast and ongoing need for consumer and patient information and education.
Challenges, Controversies, and Outlook
Sun screen should have UVB & UVA protection should be recommended, if it has only one it should be avoided.
Sunscreen of 30 SPF is 97% effective while 50 SPF Sunscreen is 98% effective, study’s have revealed.
In a recently published paper, Yarosh et al. review all publications that deal with the effectiveness of topically applied T4 endonuclease V and photolyase.
The data originate from small, little controlled studies with various endpoints (e.g., reduced formation of cyclobutane pyrimidine dimers, reduced expression of tumor protein p53, reduced number of apoptotic cells).
The nonclinical as well as the clinical data are of fundamental interest, and in view of some diseases (e.g., Xeroderma pigmentosum), the development of these enzymes as medicinal products (drug) would be of the greatest clinical interest and relevance.
Excessive solar radiation (280–800 nm) causes an increase in reactive oxygen species, resulting in oxidative stress overwhelming the antioxidative defense system of the skin. The detrimental effects of oxidative stress occur through multiple mechanisms that involve
(a) alterations to proteins and lipids, (b) induction of inflammation, (c) immunosuppression, (d) DNA damage, and (e) activation of signalling pathways that affect gene transcription, cell cycle, proliferation, and apoptosis.
(b) These alterations promote pigmentation, skin aging, and carcinogenesis.
1. User-Related Challenges:
Inconsistent or Insufficient Application: Many people do not apply enough sunscreen to achieve the labelled SPF. Studies show that users often apply only 20-50% of the recommended amount (2 mg/cm²), significantly reducing the protection. For example, if a sunscreen with SPF 30 is applied thinly, the effective SPF might drop drastically.
Infrequent Reapplication: Sunscreen needs to be reapplied every two hours, especially after swimming or sweating, to maintain its effectiveness. Many users fail to adhere to this, leading to reduced protection over time.
Skipping Application on Cloudy Days or in Winter: UV rays can penetrate clouds, and snow reflects sunlight, increasing exposure. Many people mistakenly believe sunscreen is only needed on sunny summer days. Up to 90% of UV rays can still penetrate on cloudy days.
Belief in Tanning as Protection: A tan is a sign of skin damage, not protection. It indicates that the skin has been injured by UV radiation, increasing the risk of skin cancer and premature aging.
Perceived Inconvenience: Some people find applying sunscreen time-consuming or dislike the feel and smell of certain formulations.
2. Formulation and Sensory Challenges:
White Cast: Many mineral-based sunscreens (containing zinc oxide and titanium dioxide) can leave a white or grayish cast on the skin, particularly noticeable on darker skin tones. While newer formulations use nanoparticles to minimize this, it can still be a concern for some users.
Heavy or Greasy Texture: Some sunscreens, especially older formulations, can feel heavy, greasy, or sticky on the skin, making them uncomfortable for daily use. However, many modern sunscreens are formulated to be more lightweight and cosmetically elegant.
Strong Fragrance: Some sunscreens contain fragrances that can be irritating to sensitive skin or simply disliked by the user. Opting for fragrance-free options can mitigate this.
Skin Irritation and Allergies: Certain sunscreen ingredients can cause irritant or allergic contact dermatitis in some individuals. Common allergens include oxybenzone, octinoxate, and certain preservatives or fragrances. Symptoms can range from mild redness and itching to blistering rashes. People with sensitive skin or pre-existing conditions like eczema are more prone to these reactions.
Comedogenicity: Some sunscreen formulations can clog pores and potentially lead to acne breakouts, especially in individuals with oily or acne-prone skin. Choosing non-comedogenic formulations is important for these individuals.
3. Effectiveness and Protection Spectrum Challenges:
SPF Misinterpretation: SPF primarily measures protection against UVB rays, which are the main cause of sunburn. It doesn't fully indicate the level of protection against UVA rays, which contribute to premature aging and skin cancer.
4. Environmental Concerns:
Coral Reef Damage: Certain chemical UV filters, such as oxybenzone and octinoxate, have been shown to be harmful to coral reefs, contributing to coral bleaching and DNA damage. This has led to bans on these ingredients in some locations.
Persistence in the Environment: Some sunscreen chemicals can persist in aquatic environments and may have other ecological impacts.
5. Carcinogenicity:
Some chemicals used in sunscreen are absorb 469 times of desired value, there have been studies of possible cancer casing by sunscreens , yet they are inconclusive.
Deoxyribose sugar in hair growth.
In experiments with mice suffering from testosterone-driven hair loss, daily application of Sugar Gel resulted in the regrowth of long, thick fur in the treated areas.
A study published in Frontiers in Pharmacology found that a sugar gel made from deoxyribose, a component of DNA, can stimulate hair regrowth in mice. The sugar gel, originally developed for wound healing, was found to be as effective as minoxidil, a common hair loss treatment, and even showed promise in stimulating lash and eyebrow regrowth after chemotherapy. The research suggests that deoxyribose may promote hair growth by enhancing blood flow to hair follicles.
Effective Hair Regrowth:
The deoxyribose sugar gel demonstrated significant hair regrowth in mice models of male-pattern baldness, comparable to minoxidil.
Researchers took, two group of mice, one was applied with standard minoxidil, other were applied with, used nontoxic, bio degradable sugar gel, they both showed approximately equal growth of fur.
Mechanism of Action:
The research suggests that deoxyribose may work by boosting blood supply to hair follicles, which is crucial for encouraging hair growth. The concentrate the sugar solution the better was the hair growth, the bulb becomes bigger and the hair was thicker.
Potential Applications:
The study opens up possibilities for treating various types of hair loss, including alopecia and hair loss after chemotherapy.
Biodegradable and Non-toxic:
The sugar gel is biodegradable and non-toxic, offering a potentially safer alternative to existing hair loss treatments.
This research could open ,new avenues in testosterone responsible hair loss, which have potentially no side effects.
Hair breakage


Hair breakage can be caused by a variety of factors, often related to physical, chemical, or environmental stress. Here are some common causes:
1. Heat Damage
Excessive use of hair dryers, flat irons, or curling wands can weaken hair strands.
2. Chemical Treatments
Bleaching, dyeing, perming, or relaxing hair can strip it of natural moisture and proteins.
3. Mechanical Stress
Rough brushing or combing, especially when wet.
Tight hairstyles like braids, ponytails, or buns.
4. Lack of Moisture
Dry hair is more prone to breakage. This can be due to over washing, low humidity, or not using conditioner.
5. Poor Nutrition
Deficiencies in vitamins like biotin, vitamin D, zinc, or protein can affect hair strength.
6. Over washing or Under washing
Over washing can strip natural oils, while under washing can cause buildup that weakens hair.
7. Wrong Hair Products
Harsh shampoos or products with alcohol and sulfates can dry out or damage hair.
8. Medical Conditions
Conditions like thyroid disorders, anemia, or scalp infections can contribute to breakage.
9. Environmental Factors
Sun exposure, pollution, chlorine in pools, or saltwater can all lead to hair damage.
The scalp biome


The scalp biome refers to the unique ecosystem of microorganisms (bacteria, fungi, and other microbes)
) that inhabit the scalp. This microbiome plays a critical role in maintaining scalp health, influencing hair growth, and preventing conditions like dandruff, itching, and hair loss. Below is a detailed overview of the scalp biome, its importance, and how to maintain its balance.
1. What is the Scalp Biome?
The scalp biome consists of diverse microbial communities, primarily:
- Bacteria: Dominated by Cutibacterium acnes (formerly Propionibacterium acnes) and Staphylococcus epidermidis. A healthy scalp typically has higher levels of C. acnes, while S. epidermidis is more abundant in dandruff-prone scalps.
- Fungi: Primarily Malassezia species (e.g., M. restricta and M. globosa). An imbalance in these fungi, especially an overgrowth of M. restricta, is linked to dandruff and seborrheic dermatitis.
The scalp biome is influenced by factors like genetics, diet, hygiene, stress, and environmental condition.
2. Importance of a Balanced Scalp Biome*
A healthy scalp biome:
- Protects against pathogens: Beneficial microbes outcompete harmful ones.
- Supports hair growth: Bacteria like C. acnes contribute to nutrient production (e.g., biotin and B-vitamins) essential for hair follicles.
- Maintains scalp pH: A slightly acidic pH (4.5–5.5) helps preserve microbial balance.
- Prevents scalp conditions: Dysbiosis (imbalance) can lead to dandruff, itching, inflammation, and even hair loss.
3. Signs of an Unbalanced Scalp Biome
Common symptoms include:
- Flaking or dandruff.
- Itching, redness, or irritation.
- Excessive oiliness or dryness.
- Hair thinning or shedding.
4. How to Maintain a Healthy Scalp Biome*
a) Gentle Cleansing*
- Use sulfate-free shampoos to avoid stripping natural oils and disrupting the microbiome.
- Wash hair 2–3 times weekly to prevent over-drying or oil buildup.
b) Probiotic and Prebiotic Care
- Probiotic shampoos or serums can reintroduce beneficial bacteria.
- Prebiotic ingredients (e.g., rosebay extract) nourish good microbes.
c) Natural Oils and Treatments
- Coconut oil has been shown to increase C. acnes and M. globosa, improving scalp health.
- Tea tree oil has antifungal properties but should be diluted to avoid irritation.
d) Diet and Lifestyle
- Eat fermented foods (yogurt, kimchi) to support gut and scalp health.
- Reduce stress, as cortisol imbalances can disrupt the microbiome.
e) Avoid Harsh Chemicals
- Limit heat styling, chemical treatments, and products with alcohol or sulfates.
5. Professional vs. DIY Care*
- Professional treatments (e.g., dermatologist-prescribed antifungals) are effective for severe imbalances.
- DIY care (e.g., scalp massages, gentle exfoliation) works for maintenance.
Hidradenitis suppurativa


Hidradenitis suppurativa (HS), also known as acne inversa, is a chronic disabling and debilitating inflammatory disease with high unmet medical need. The estimated prevalence of HS is 1–2% globally.
The prevalence of HS is likely to be under-reported and further hindered by under-diagnosis. Disease onset typically occurs in early adulthood, although late-onset disease can occur, and delayed diagnosis is common, with a reported average delay of 10 years between the initial manifestation of symptoms and diagnosis.
HS can be mild to severe: early initiation of the disease involves hair follicle alterations with folliculitis and peri folliculitis, which can lead to persistent, deep-seated nodules and abscesses affecting the axillae, groin, buttocks and other intertriginous skin areas.
Neoepithelialized tunnels are a unique morphological feature of late-stage HS that form in the dermis and can connect with the skin surface, releasing purulent discharge. Draining tunnels are increasingly recognized as a source of inflammation and as active mediators of disease pathogenesis.
Over time, chronic uncontrolled inflammation results in irreversible tissue destruction and scarring.
HS has profound, wide-ranging, negative consequences for patients, including chronic pain, mobility deficits, depression and anxiety, suicide and suicidality, stigmatization, impaired body image and sex life, unemployment and socio-economic consequences.
Moreover, the high frequency of comorbidity and concomitant disease in HS, in particular metabolic syndrome, which is observed in approximately 40% of patients from an early age,24 contributes to increased cardiovascular disease and morbidity and a reduction in life expectancy.
The exact cause of HS is unknown, but it is a complex disease with contributory genetic and epigenetic changes, and hormonal, mechanical, microbial and lifestyle factors such as obesity and smoking.
Multiple immunological pathways are involved, with a variety of different cells and their soluble mediators. Despite the incapacitating nature of HS, the treatment landscape is limited, leading to inadequate management of the disease for many patients.
Current treatment options to reduce symptom burden include topical antibiotic treatments (e.g. clindamycin), local steroid injections, systemic therapies (including high-dose oral zinc gluconate), and repeated and/or rotational courses of systemic antibiotics (e.g. tetracycline, clindamycin and Rifampin), retinoids (acitretin) and hormonal therapies (metformin and antiandrogens).
Various physical/surgical procedures exist (e.g. incision and drainage, deroofing, ablative CO2 laser local and wide excision), with guidelines generally recommending concomitant use of both surgical and medical treatments, particularly in advanced HS with irreversible lesions.
However, recurrence following surgery is not uncommon and is procedure dependent. Therefore, targeting the early inflammatory phase of HS is considered to be a core element of disease management to prevent onset.
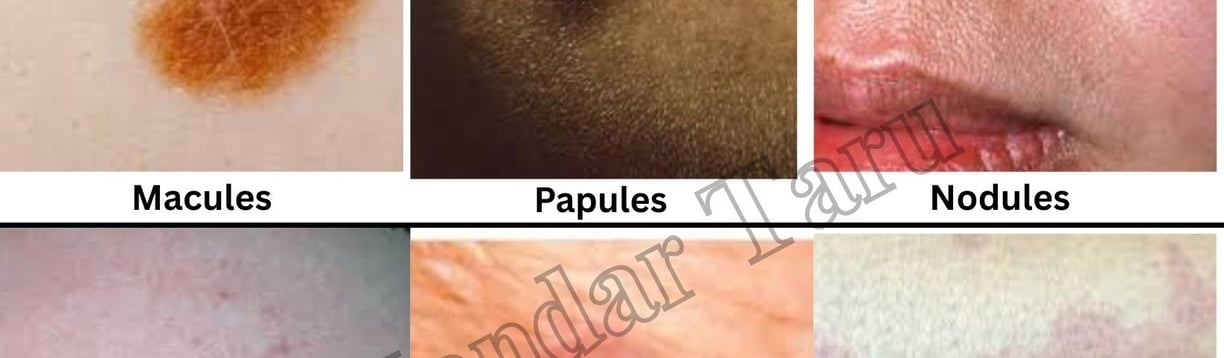
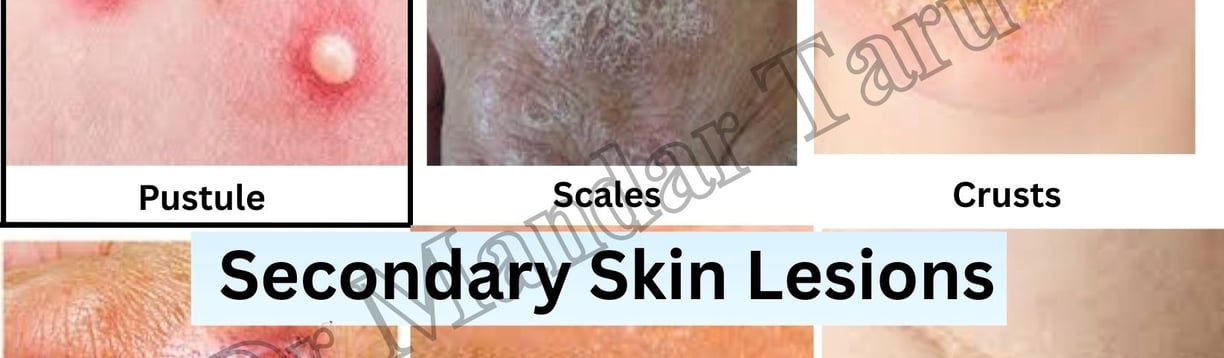
Skin Lesions